What is Proactive Pharmacy Claims Management?
In the member services industry being proactive instead of reactive makes an enormous impact. It makes a great difference in level of service of any industry but is especially important in health care. Health care services are detrimental to the livelihood of patients. MedalistRx is a proactive Pharmacy Benefit Manager.
We live in a world where nearly all of the customer service industry is reactive and slow to assist, MedalistRx believes this needs to change. At MedalistRx our member services team is proactive in pharmacy claims management. Proactive member service helps in several ways, here are a few:
Correcting Input Errors
At times prescriptions may reject due to errors such as a pharmacy inputting incorrect processing information, DOB, gender codes, or packaging errors. When our team recognizes a pharmacy error they make an outbound call to help with a correction. Often pharmacy errors are resolved prior to a member ever noticing the initial rejection.
Cost Savings
Physicians sometimes write a prescription using the brand name when a lower cost generic medication is available. MedalistRx member services is knowledgeable and able to recognize when a lower cost generic is available versus the name brand medication written by the physician. Our member services team proactively reaches out to request generic. This process helps to save both members and our clients significantly and helps MedalistRx clients maintain one of the best generic utilization rates in industry.
Copay Assistance Programs
Sometimes a brand medication is the best option for treatment. Brand medications can be expensive, so manufacturers provide copay assistance to help lower the out of pocket (OOP) cost to patients. MedalistRx member services team is knowledgeable on brand copay card programs. When a brand medication is processed; our team members reach out to the pharmacy to ensure a copay card is being used. This extra step significantly saves both our members and clients on brand medications.
Account Management
Specialty medications are used to treat rare disease categories and can be very expensive. Specialty drugs can cost as much as $30,000 per month. These medications always require a prior authorization (PA). Our member services team reviews claims in real time. When a specialty medication rejects for PA our Account Managers proactively reach out to clients to provide treatment information and possible cost implications. This communication provides a proactive alert to clients to help effectively manage the highest cost medications on their plan
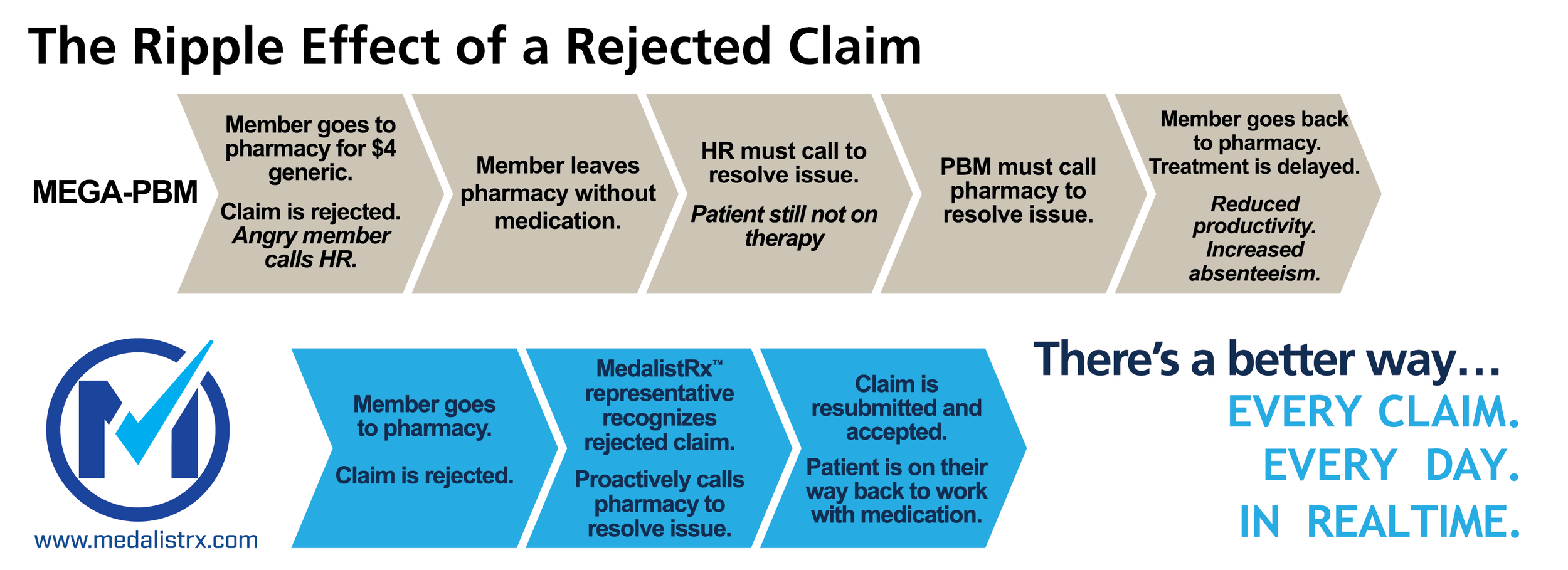
Tracking pharmacy claims in realtime makes an impact
Our team has human eyes on every prescription that rejects and assists proactively with resolving rejections. In a 2020 study we found our member services team proactively tracked and resolved 12,132 prescription claims errors
These 12,132 patient prescriptions processed without error because MedalistRx pharmacy benefit management (PBM) delivers results. A standard PBM would have members and clients doing the work of resolving a rejection, instead of the PBM they assigned to manage their prescriptions. Our process is simple yet highly effective.
“Employer sponsored health plans drastically need an innovative
Pharmacy Benefit Manager (PBM) to manage pharmacy claims, instead
of simply processing them.
Our proactive approach to pharmacy claims management guarantees our members receive the absolute best
member services experience at the lowest possible price.”